Meniere’s Disease
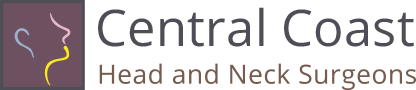
Endolymphatic hydrops and Meniere’s disease are disorders of the inner ear. Although the cause is unknown, it probably results from an abnormality of the fluids of the inner ear. In most cases, only one ear is involved but both ears may be affected in up to 20% of patients.
The Symptoms
A patient with endolymphatic hydrops may experience any combination of the below described symptoms:
Vertigo is the most troublesome symptoms of endolymphatic hydrops. The vertigo of endolymphatic hydrops may occur in attacks of a spinning sensation which may result in nausea and sometimes vomiting. The vertigo may last for as short as a few minutes or as long as hours. During attacks the patient is usually unable to perform activities normal to their work and home life. Sleepiness may follow for several hours and an off-balance sensation may last for days following an attack. Some patients do not have attacks of spinning vertigo but have episodes of disequilibrium in which their head may feel as if it is swimming or the floor seems to be shifting beneath their feet.
There may be an intermittent hearing loss during the disease, especially in the low pitches, but a fixed hearing loss involving tones of all pitches commonly develops in time. It is not uncommon for loud sounds to be very uncomfortable and to appear distorted in the affected ear.
The excessive fluid pressure on the hearing nerves may also cause tinnitus. The tinnitus of endolymphatic hydrops may sound like crickets or a high tone but most commonly sounds like a low-pitched hiss which may increase and decrease in intensity as the fluid pressure increases and decreases.
The increased fluid pressure in the inner ear may also result in a sensation of fullness or pressure within the ear which cannot be cleared by popping the ear.
The symptoms of endolymphatic hydrops may be only a minor nuisance or can become disabling especially if the attacks of vertigo are severe, frequent, and occur without warning. In patients who have all of the above-described symptoms, we apply the term Meniere’s disease after the French otologist Prosper Meniere who first described this inner ear syndrome in 1856
Watch an animation depicting the fluctuating symptoms of Meniere’s disease.
How is a Diagnosis of Endolymphatic Hydrops Made?
The diagnosis of Meniere’s disease is usually made by identifying the cardinal symptoms of ear fullness, fluctuating hearing loss, episodic vertigo and characteristic roaring or seashell tinnitus. In addition to a history and physical examination you will be asked to undergo some diagnostic studies to rule-out causes for your symptoms other than an inner ear disorder. This may take the form of blood tests, hearing tests, x-rays, CT scans or MRI scans of the brain and inner ear or electrocochleography.
Perhaps the most important testing for any patient with Meniere’s disease is serial audiometry. An audiometric examination (hearing test) is performed to look for characteristic types of hearing loss in the affected ear. Because the hearing can change from day to day in patients with Meniere’s disease, audiograms on sequential visits are obtained to look for signs of fluctuating hearing levels that are characteristic of Meniere’s disease. Speech discrimination (the ability to distinguish between words like “sit” and “fit”) is often diminished in the affected ear and is also tested for. Tympanometry is also performed in order to determine if pressure symptoms could be originating from the middle ear rather than the inner ear.
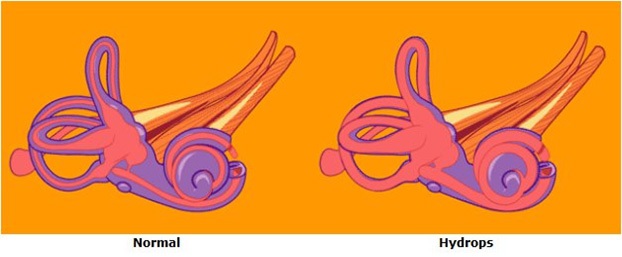
Electrocochleography may indicate increased inner ear fluid pressure in some cases of endolymphatic hydrops. In this test a tiny electrode is placed in the ear canal near the inner ear. The tiny electrical impulses from the hair cells of hearing in the inner ear are then recorded and characteristic changes which are seen in conditions of inner ear pressure are looked for.
An ENG ( electronystagmography) and VEMP (vestibular evoked myogenic potentials) exam may be performed. Just as the hearing test measures the function of the hearing nerve endings, the ENG and VEMP measure the strength and function of the nerve endings in the balance end of the inner ear. With time, the balance function in an ear with Meniere’s disease will decrease and the intensity of vertigo will decrease. The ENG is done in a darkened room. Recording electrodes are placed near the ears. Wires from the electrodes are attached to a machine similar to a heart monitor. Warm and cool water are gently introduced into each ear canal. Since the eyes and ears work in a coordinated manner through the nervous system, measurement of eye movements can be used to test the balance system. In about 50% of patients the balance function is reduced in the affected ear. Other balance tests such as rotational testing or balance platform tests may also be performed to evaluate the balance system.
Computed Tomography (CT scanning) or magnetic resonance imaging (MRI) may be needed to rule out other causes of some of the symptoms the patient is experiencing before they can be attributed to endolymphatic hydrops.
How Can Meniere’s Disease Be Treated?
The cause of Meniere’s disease is still unknown. Recent research suggests disorders of maintenance of the ion balance in the inner ear fluids may be the root cause of the ear symptoms in Meniere’s disease. The inner ear in patients with Meniere’s disease is often ill because of an outside aggravating factor, such as allergy, typical or atypical migraine, temporomandibular joint or neck problems. If the cause of the irritation to the inner ear can be identified in a patient, avoiding and treating that cause are often more fruitful than concentrating on the ear symptoms themselves. Treatments may involve medication, extensive diet changes, lifestyle changes, introduction of drugs to the inner ear, and surgery.
In patients with no identifiable cause for their Meniere’s disease, a low salt diet and diuretic (water pill) may reduce the frequency and severity of symptoms. In order to receive the full benefit of the diuretic it is important that you restrict your intake of salt to less than 1500milligrams/day and take the medication regularly as directed. Please buy a nutrition handbook that can help you learn which foods we commonly eat that are loaded with salt. Not all foods that are loaded with salt taste salty!
If you are experiencing prominent balance symptoms from your endolymphatic hydrops, antivertigo medications such as Antivert (generic name: Meclizine) or Valium (generic name: Diazepam) may be prescribed to provide temporary relief during episodes of disequilibrium. If balance symptoms are prominent in your case, you will learn to adjust your medication to the degree of symptoms caused by the swelling of your ears at any particular time. The use of these medications is generally not a good long-term strategy but can allow you to continue to function while more effective treatments are explored.
Fludrocortisone is an effective medication for many patients with Ménière’s disease. It has long been known that the inner ear responds well to sugar steroids called glucocorticoids, but they are not a workable long-term medication because of long term steroid side effects. Many ears with Meniere’s disease respond to a mineral steroid, fludrocortisone, which is well tolerated in patients with normal blood pressure, kidney and cardiac function. Fludrocortisone helps the inner ear so much that patients do better even though the medication causes them to retain salt.
Meniere’s Disease and Migraine
There is increasing interest among ENT physicians in the connection between migraine and Meniere’s disease. While the prevalence of migraine in the US population is 13%, the prevalence of migraine in patients with Meniere’s disease is 56%, and the prevalence of migraine in patients with bilateral Meniere’s disease is 85%.
We have recently discovered that the tiny blood vessels in the inner ear are innervated by branches of the same nerve that innervates the intracranial blood vessels severely affected in migraine attacks. Electrical stimulation of this trigeminal nerve has caused fluid changes in the inner ear which could affect it severely enough to cause a problem like Meniere’s disease. Many patients with migraine and Meniere’s disease who are treated effectively for migraine have experienced an improvement in their Meniere’s symptoms.
This animation shows blood flow changes and the extravasation of inflammatory substances usually associated with migraine occurring in the inner ear. Changes in the membranous labyrinth also occur. There is increasing evidence to support this migraine mechanism of Menieres disease.
For more information about migraine.
Inner Ear Perfusion With Steroids
In most patients, the activity in the affected ear responds well to steroids taken orally. Oral steroids, however, provide only temporary relief and have other physiologic consequences that make them unacceptable for long term treatment. Success in controlling symptoms has been achieved by introducing high doses of steroids directly to the inner ear. This procedure, called Dexamethasone Perfusion avoids the systemic effects of oral steroids. The procedure is simple and safe. The eardrum is viewed under the operating microscope and small spots are numbed with anesthetic applied with a tiny Q-tip. The middle ear is then filled with a solution of steroid in a way that it will contact the membranes of the inner ear. This treatment may give decreased symptoms for months or years and can be repeated easily because the patient can go directly to work on the same day as their perfusion.
Inner ear Perfusion. This illustration shows medication filled into the middle ear diffusing into the labyrinth.
Labyrinthectomyis a procedure which is recommended for those individuals who have no residual hearing in the affected ear. In this operation the inner ear is removed through an incision behind the ear. This results in a 95% rate of control of vertigo attacks. Recovery may take three to six weeks depending on the age of the patient and the demands of their occupation.
Inner Ear Perfusion With Gentamycin
Injections of the antibiotic Gentamicin through the eardrum (Gentamycin Perfusion) can be done in the office to weaken the balance nerve endings in the inner ear so that they cannot cause such severe attacks of vertigo. This medication is much more toxic to the balance nerve endings than the hearing nerves so it can be used in patients with good hearing with acceptable risk. This procedure offers good control of vertigo without any of the risk of general anesthesia or the expense of hospitalization. A weeks long recovery period is typical during which the patient will perform exercises designed to teach the brain to function with one weak labyrinth.
Most patients find that their attacks after gentamycin perfusion are milder and easily managed without impairing their ability to function at their work or inconvenience them. If the attacks are still too strong, a second perfusion can be given, with milder recovery. In our clinic 80% of patients find a single perfusion adequate. Gentamycin perfusion is also referred to as Chemical Labyrinthectomy.
Other operations or treatments may be advised in particular cases. If surgical treatment is necessary, the risks and benefits of surgery will be thoroughly discussed with you. There is no surgical treatment to improve hearing loss or tinnitus associated with endolymphatic hydrops.
Migraine - More than a Headache
Introduction
Migraine is a common clinical problem characterized by episodic attacks of head pain and associated symptoms such as nausea, sensitivity to light, sound, or head movement. It is generally thought of as a headache problem, but it has become apparent in recent years that many patients suffer symptoms from migraine who do not have severe headaches as a dominant symptom. These patients may have a primary complaint of dizziness, of ear pain, of ear or head fullness, “sinus” pressure, and even fluctuating hearing loss. Fortunately, treatment regimens long established for the treatment of “classic” migraine headaches are generally effective against these “atypical” symptoms of migraine.
How Common is Migraine?
There are currently 28 million Americans with “classic” migraine headaches. In a room with 100 people, 13 are likely to have migraine. This is as common as diabetes and asthma combined. The number of people suffering with atypical forms of migraine is unknown. Females are 3 times more likely to have migraine than males. Although any person can have migraine at any age, migraine is most common between ages 30 and 50. The peak incidence of migraine in females occurs at 35 years of age - at this age, 28% of all females have migraine headaches. The peak incidence of migraine in men occurs at 30 years of age - at this age, about 10% of all males have migraine headaches.
Migraine is a lifelong problem. It may start in childhood and disappear and reappear in new forms throughout an individual’s life. In general, there is a decrease in headache intensity and an increase in the incidence of atypical symptoms of migraine (vertigo, ear pain, bowel symptoms, etc.) as patients mature.
Surveys show that only 48% of people with migraine headaches have had a diagnosis and are being treated for their headaches. Unfortunately, only 29% of US migraine sufferers are very satisfied with their treatment. This is usually a reflection of a lack of understanding of the nature of migraine and its treatment, or lack of commitment to effective treatments. We hope this material will help you to achieve better control of your migraine symptoms, whatever they are, and improve your quality of life.
How are People with Migraine Different?
Migraine is an inherited problem of ion channels in the brain. This may result in what is best described as a “sensitive brain”. Most individuals exposed to loud noise, bright light, or excessive motion can adapt to these strong stimuli within minutes, but in the brain of a migraineur, the strength of the stimulus continues to grow until a migraine crisis occurs. This lack of ability to adapt to strong sensory stimulation helps us understand why so many patients have migraine headache or other migraine symptoms that can be provoked by bright light, excessive noise, strong smells, excessive motion, and painful stimuli.
What Happens During a Migraine Attack?
Abnormal activity may occur in, on, and around the brain during a migraine attack. Hyperactivity deep in the brainstem and other brain centers that control pain and other sensations in the head has been found on brain imaging studies in patients having migraine attacks. This means a person having a migraine who senses pain, motion, or sound will tend to have an exaggerated, distorted experience of the pain, motion, or sound that may be so intense that it is difficult to tolerate. The patient may become so sensitive that he has no choice but to withdrawal to a quiet, dark place and sleep until the episode has passed. Other symptoms of migraine deep in the brain may include nasal congestion, retention of fluid, lethargy, nausea, fainting, anxiety, fever, and even seizures.
Patients also have altered electrical activity at the surface of the brain during a migraine episode. This most commonly occurs over the vision areas of the brain and may result in unusual visual phenomena such as the appearance of spark-like bursts, wavy lines, blind spots, or even complete visual loss in rare cases. Abnormal cortical brain activity over other regions of the cortex can result in temporary confusion, inability to speak, numbness, or even paralysis of any part of the body. These symptoms which occur at the surface of the brain typically are brief, lasting no longer than 20 minutes.
Painful throbbing headache may be associated with sensitization of the blood vessels around the brain by abnormal chemicals which themselves irritate and cause the blood vessels to hurt.
What is a Migraine Trigger?
A migraine trigger is any environmental, dietary, or physiologic factor that can provoke migraine activity in the brain.
Environmental triggers
Examples of environmental triggers include odors, bright lights, noise, and other excessive sensory stimuli. Painful stimuli that trigger migraine usually occur in the head and neck. The most common of these are neck injury and spasm, temporomandibular joint pain, and sinus pain. 40% of migraineurs are affected by weather changes. The mechanism of this trigger is not currently understood.
Food triggers
There are hundreds of potential food triggers for migraine. Comprehensive lists of foods which may contribute to triggering migraine can easily be found on the Web. In general, these foods fall into two main categories: 1) byproducts of food aging and 2) foods with chemicals similar to neurotransmitters our brains use. Byproducts of food aging are found in fermented products like red wine, aged cheeses, and yeast in fresh bread and yogurt. Foods with chemicals similar to our own neurotransmitters which may aggravate migraine are coffee, chocolate, MSG, and the nitrates used as preservatives in many of our prepackaged foods. Food triggers are not the result of allergy, but are direct chemical sensitivities.
There is a common misconception that if a person is sensitive to a food item, they will know it, because they will have migraine symptoms within an hour of eating the particular food item. In fact, some effects may come immediately or sometimes days later. Added to this confusion is the reality that many real food triggers may not cause migraine alone, but only in combination with other partial triggers, which together may provoke an attack of migraine headache or symptoms. For example, some migraineurs can eat chocolate or red wine alone with no problem, but will suffer a migraine attack if chocolate and red wine are taken together. We generally recommend an initial dietary trial which avoids only the most common migraine triggers. If good results are not achieved within a few weeks, a comprehensive diet which eliminates all potential migraine triggers is recommended. It may take 6-10 weeks for a patient suffering from severe and debilitating migraine symptoms to respond, but most do. After an improvement in symptoms is achieved, suspect foods can be added to the diet one at a time to see whether they are an important trigger for that patient. Despite the difficulty of this kind of a trial, we have found that even the most severely affected migraineurs tend to respond and are generously rewarded for their efforts.
To see a comprehensive list of common food triggers for migraine, click here. This list can be printed and lists all foods in alphabetical order, so it is easy to use in the supermarket.
Physiologic triggers
Perhaps the most common trigger of migraine is stress. Patients commonly report increased symptoms when they are fatigued and suffer lack of sleep. Many other physiologic stresses can also trigger migraine, such as hunger, exercise, and pain. Some patients suffer migraine from sleeping too much, and cannot understand why most of their weekends are ruined by headaches or dizziness. Migraines are commonly triggered by hormone changes, like the drop in estrogen levels before the menstrual period or after menopause.
Subtle physiologic stresses, like eye strain, can trigger migraine. It is not uncommon for someone with new-onset headaches to find their eyeglass prescription has changed. Updating the prescription can have dramatic positive results. You will be asked to consider an eye examination if other obvious triggers are not identified.
Other common physiologic triggers include pain from temporomandibular joint dysfunction, neck problems, and sinusitis. Treatment of these underlying problems can result in dramatic reduction in typical and atypical migraine symptoms.
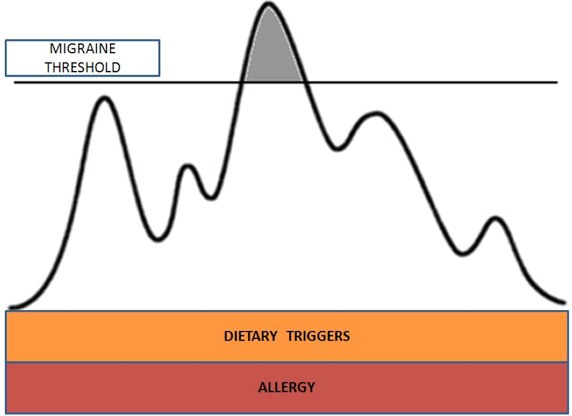
As can be seen in the figure below, environmental, physiologic and dietary triggers may add up in different ways on different days. When the migraine threshold of the individual is surpassed headache or other migraine related symptoms may occur. Elimination of any trigger such as dietary triggers and allergy (show here) can give more room for other less controllable triggers such as stress and weather change to add up before crossing the migraine threshold. Reducing the trigger load commonly results in less frequent and less severe breakthrough symptoms.
Treatment of Migraine
It seems easy to take pain medications or abortive medications such as narcotics or triptans to suppress symptoms, but when taken frequently, these can worsen the problem by causing rebound symptoms more intense than the original attack. It is typical for patients to get themselves into a vicious cycle, resulting in decreased functioning at work and at home with the expected emotional consequences before treatment is sought. The best treatment results will be obtained by those patients who work to understand what migraine is and how migraine is affecting their lives. This allows a teamwork approach with the physician and better outcomes.
The mainstay of treatment for migraine headache and atypical migraine symptoms is trigger identification and avoidance. This requires education about migraine triggers and the use of a migraine diary in which the patient is asked to record their symptoms and the probable trigger for that particular episode. Unlike many environmental and physiologic triggers, dietary triggers can be avoided. In general, an attempt to improve lifestyle by reducing stress, improving sleep habits, and adding regular exercise are beneficial. When done maximally, many patients will obtain near complete freedom from their migraines with this treatment alone.
At times, symptoms may be so constant that individual events and their triggers cannot be easily identified. In these cases, it may be helpful to give medications to elevate the threshold above which migraine triggering in the brain occurs. These may be medications originally used for blood pressure control, depression, or seizures which have been found to be easily tolerated and very good at preventing frequent migraine attacks. When this is successful, the breakthrough attacks which do occur are usually easily attributed to some particular trigger or aggravating factor, which can then be avoided. It may take 6-8 weeks to respond to a medication, and it is not uncommon for a patient to have to try more than one medication. Patients requiring medications to elevate migraine threshold can realistically expect a 50-80% reduction in symptom intensity and frequency.
If after maximizing the benefits of trigger identification and avoidance and medications to elevate the threshold of migraine, breakthrough headaches are still occurring, medications to abort acute attacks may be prescribed. There are now excellent medications which can help improve migraine symptoms both deep in the brain and those painful symptoms associated with sensitized blood vessels around the brain. These new medications are called triptans. Because they can cause rebound, they should not be used more than 6-8 times a month. Doctors’ opinions may vary on this.
Some patients will have occasional severe headaches which can be aborted effectively with triptans without the risk of rebound. These patients should always be on the lookout for an increase in headache frequency and intensity that are the first signs of rebound. Long term treatment of acute headaches with narcotics generally leads to increasing medication needs and must be considered very cautiously, especially in patients with histories of chemical dependency.
How to Keep a Migraine Diary
Keeping a simple diary may be one of the most important tools you and your physician have for making treatment decisions. It is not necessary to keep extensive notes. In fact, the simpler the record keeping, the better. Use a monthly calendar, preferably a small one, like a checkbook calendar which you can keep with you. Use two pencils or pens of different color. With one color, mark the days you have headaches. With the other color, mark the days you have dizziness or symptoms other than headache (e.g., lethargy, head fullness, ear pain). Make a note of any possible physiologic, dietary, or environmental triggers that have been present in the 24 hours prior to your symptoms. Remember to bring your diary with you to your appointments. It will allow you and your physician to see your progress at a glance.
Unusual Forms of Migraine
As you understand by now migraine is more than a headache. It is a constellation of symptoms and headache is not necessarily an essential part. It is extremely important to acknowledge this because although these atypical symptoms of migraine generally do not respond to abortive medication like the pain of a migraine headache does, the atypical symptoms can be managed by careful identification and avoidance of triggers or by taking medication for prophylaxis of migraine. These migraine symptoms which are not headaches but which are aggravated by typical migraine triggers are sometimes referred to as migraine equivalents. Some more common forms are mentioned here.
Cyclical vomiting is generally seen in childhood but may continue into adult life in some cases. The attacks are characterized by recurrent episodes of vomiting every 10-15 minutes and which typically continues for hours after the episode is triggered. There is no headache. Other patient’s may experience abdominal migraine which presents as a pain in the upper central abdomen. The common stomachache of childhood is more likely to be caused by migraine than ingestion of foods which directly irritate the stomach. Periodic diarrhea, like cyclical vomiting, has symptoms most manifested as recurrent noninfectious diarrhea. These patients often undergo extensive abdominal and intestinal workups for infection or other intrinsic diseases of the bowel which are negative. It is not unusual for our successfully treated migraine patient’s to have such an improvement in their abdominal symptoms that they are able to discontinue medications they have been taking chronically for a diagnosis of irritable bowel syndrome. Migraine can also be the cause of spontaneous high fevers. This is especially common in children who may have no sign of infection that can be identified by their pediatrician. Many cardiologists and Emergency Room personnel have encountered patient’s with chest pain who have no changes on the EKG and whose pain does not respond to antacid medication. These patients’ with precordial migraine become well known to their physicians because their atypical episodes disappear when they begin taking medications for prophylaxis of migraine. Migraine equivalents may also manifest as dramatic mood changes particularly in the form of hyperactivity or irritability or an overwhelming tendency to very deep sleep that is often diagnosed as narcolepsy. It is not uncommon for women to experience some of these migraine equivalent symptoms as a portion of their premenstrual syndrome. Other migraine equivalents such as vertigo, Meniere’s disease, recurrent Benign Paroxsymal Positional Vertigo, otalgia “ear pain” and sinus pressure are seen with particular frequency by otolaryngologists and are described separately below.
Migraine and Inner Ear Disease
There is increasing interest among specialists in possible associations between migraine and inner ear disease. Because the blood vessels of the inner ear are enervated by branches of the same nerves that enervate the blood vessels of the brain associated with migraine headache, the inner ear may suffer from its own ear specific migraine attacks. The character of the ear symptoms may reflect temporary changes in normal inner ear function with symptoms that come and go or longer lasting symptoms from injury to the delicate inner ear from migraine related vascular changes or the release of inflammatory mediators. Migraine related ear symptoms may vary from patient to patient and may take the form of episodic vertigo, benign paroxysmal positional vertigo(Benign Paroxsymal Positional Vertigo), recurrent benign positional vertigo, Meniere’s disease, ear pain, aural pressure, tinnitus, fluctuating hearing loss, and sudden hearing loss. Awareness of these possible associations is important because symptoms often respond to migraine treatments. A trial of migraine treatment should be considered if a current or even a past migraine history is present, especially if a destructive surgical procedure is contemplated. Below are some patient interviews with patients who have had various inner ear symptoms not usually associated with migraine but whose symptoms improved with migraine treatment.
Migraine and Meniere’s Disease
There is increasing interest among ENT physicians in the connection between migraine and Meniere’s disease. Meniere’s disease is a disorder of the inner ear characterized by episodic fullness, tinnitus (ringing), hearing loss, and vertigo whose cause is poorly understood. While the prevalence of migraine in the US population is 13%, the prevalence of migraine in patients with Meniere’s disease is 56%, and the prevalence of migraine in patients with bilateral Meniere’s disease is 85%.
We have recently discovered that the tiny blood vessels in the inner ear are innervated by branches of the same nerve that innervates the intracranial blood vessels severely affected in migraine attacks. Electrical stimulation of this trigeminal nerve has caused fluid changes in the inner ear which could affect it severely enough to cause a problem like Meniere’s disease. Many patients with migraine and Meniere’s disease who are treated effectively for migraine have experienced an improvement in their Meniere’s symptoms.
For more information about Meniere’s disease.
Migraine and Vertigo
25% of migraineurs experience vertigo along with their other migraine symptoms. In many patients seen at our balance center, vertigo is the predominant feature of their migraine. We typically find that they have had more classic migraine headaches at some time in the past, or have a family history of migraine. Migraine symptoms of new onset in a patient with no personal or family history of migraine can also occur. This is particularly common after head injury or whiplash with chronic neck symptoms. Neck symptoms and spasm tend to increase weeks to months after an initial whiplash injury, causing headache and associated episodes of vertigo. These symptoms are generally not associated with pressure in the ear or hearing changes and may originate in the brainstem from faulty central processing of balance information from the inner ears. This may explain why many patients with migraine associated vertigo do not respond to vestibular suppressant medications such as meclizine or diazepam, which work only in the inner ear and vestibular nerves, but not in the brainstem. These patients are often best treated with physical therapy to decrease neck muscle stiffness and pain, medications to decrease neck muscle stiffness and pain, as well as traditional migraine therapy.
Most migraineurs have a lifelong history of motion sickness and can relate a history of motion intolerance that includes car-sickness, sea-sickness, or an inability to tolerate amusement park rides. A new onset of motion intolerance in an adult is more commonly associated with migraine activity than any other vestibular disorder.
Migraine and Otalgia (Ear pain)
Up to 40% of migraineurs report sharp ear pains which last only seconds. These may occur infrequently and spontaneously between migraine headaches. Ear pain has many causes, including infection and Eustachian tube problems in the ear, TMJ, and referred pain from the extensive lining of the throat. Migraineurs who present to the doctor with ear pains frequently complain that their ears are hypersensitive to touch, to wind, and to cold. When an otolaryngologist has ruled out all of these other causes of ear pain in a patient with a history of migraine, migraine treatment is often effective in eliminating the pain.
Migraine and Sinus Pressure
A great deal of confusion exists among patients and their physicians regarding the source of symptoms of facial pressure. While facial pressure is indeed a cardinal symptom of sinusitis, up to 45% of migraine patients report attack-related “sinus” symptoms, including tearing, runny nose, and nasal congestion. In migraine, these symptoms are caused by a strong outflow of nerve signals normally associated with migraine, but which causes swelling of the mucous membranes in the nasal cavity and sinuses. These symptoms may last only a few minutes or hours during the migraine episode. Sinus symptoms caused by colds or sinus infections tend to last for days.
Sinus pain, which feels like pressure, is also commonly associated with migraine, and may be the only “headache” experienced in a migraine. In migraine, symptoms tend to last minutes to hours rather than for days, as in sinus infections. 50% of migraine patients report that their headaches are influenced by weather.
Migraine and Patent Foramen Ovale
There is increasing interest in the relationship between migraine and patent foramen ovale (PFO). The foramen ovale is a hole in the heart important to our circulation before we are born and breathe air. After birth, the hole normally closes. In some individuals, it may stay partly open (patent foramen ovale). Patent foramen ovale is more common in migraineurs with aura, and migraine with aura is more prevalent in patients with PFO. Migraineurs with and without aura may derive significant benefit from PFO closure, but to date no prospective, randomized study to confirm this has been completed.
Botox and Migraine
Botox is a paralyzing agent used by doctors to decrease muscle activity. Many patients with migraine who have failed treatment with standard therapies respond to injections of Botox into the scalp muscles and sensitive areas of the scalp. Despite its effectiveness, the uncomfortable injections need to be repeated every 8-12 weeks. Few patients require Botox for migraine control.
Where can I Learn More about Migraine?
Beyond these brief pages, I typically recommend that my patients read the book, Heal your Headache the 1-2-3 Program by David Buchholz, MD. This book provides a comprehensive diet plan composed completely of foods that do not trigger migraine. It is much easier to follow this diet than to be suspicious of every food of every food you have in your cabinet at home or that you see in the supermarket. It also teaches and emphasizes the concepts of rebound and the additive character of migraine triggers. Patients who have severe migraine-related vertigo may not be able to read a whole book because of their condition. They will benefit greatly from reading the book together with a family member who can help them to stay on track and to understand all the concepts in the book.
Those patients who do love to read and who have very atypical manifestations of migraine often find great comfort in the experiences of Oliver Sacks, MD, in his book, Migraine. Dr. Sacks is an extremely insightful neurologist with a gift for writing and who himself had migraine at age 2. He has collected an astonishing series of patient stories with both common and extremely unusual symptoms, all attributable to migraine mechanisms.
Association of Migraine Disorders http://www.migrainedisorders.org/
References
- Lipton RB, Stewart WF, Diamond S, et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41(7):646-657.
- http://www.cdc.gov/nedss/
- http://www.arthritis.org
- http://www.census.gov
- Lipton RB, Stewart WF. Migraine in the United States: a review of epidemiology and health care use. Neurology. 1993;43 (suppl 3):S6-S10.
- Stewart WF, Linet MS, Celantano DD, et al. Age- and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiology. 1991;134:1111-1120.
- Lipton RB, Stewart WF, Simon D. Medical consultation for migraine: results from the American Migraine Study. 1998;38:87-96.
- Lipton RB, Scher AI, Kolodner K, et al. Migraine in the United States: epidemiology and patterns of health care use. 2002;58(6):885-894.
- Vinson DR. Treatment patterns of isolated benign headache in US emergency departments. Ann Emerg Med. 2002;39(3):215-222.
- Lipton RB, Stewart WF. Acute migraine therapy: do doctors understand what patients with migraine want from therapy? 1999;39 (suppl 2):S20-S26.
- Lance JW, Goadsby PJ. Mechanism and Management of Headache. London, England: Butterworth-Heinemann; 1998.
- Silberstein SD, Lipton RB, Goadsby PJ. Headache in Clinical Practice. 2nd ed. London, England: Martin Dunitz; 2002.
- Olesen J, Tfelt-Hansen P, Welch KMA. The Headaches. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2000.
- Honkasalo ML, Kaprio J, Winter T, et al. Migraine and concomitant symptoms among 8167 adult twin pairs. Headache. 1995;35:70-78.
- Ophoff RA, Terwindt GM, Vergouwe GM, et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. 1996;87:543-552.
- May A, Ophoff, RA, Terwindt GM, et al. Familial hemiplegic migraine locus on chromosome 19p13 is involved in common forms of migraine with and without aura. Hum Genet. 1995;96(5):604-608.
- Nyholt DR, Lea RA, Goadsby PJ, et al. Familial typical migraine: linkage to chromosome 19p13 and evidence for genetic heterogeneity. 1998;50:1428-1432.
- Peroutka SJ, Wilhoit T, Jones K. Clinical susceptibility to migraine with aura is modified by dopamine D2 receptor (DRD2) NcoI alleles. 1997;49:201-206.
- Welch KM, D’Andrea G, Tepley N, et al. The concept of migraine as a state of central neuronal hyperexcitability. Neurol Clin. 1990;8(4):817-828.
- D’Andrea G, Cananzi AR, Joseph R, et al. Platelet excitatory amino acids in migraine. 1989;9 (Suppl 10):105-106.
Migraine in One Minute
Food Awareness for Migraine
Introduction
It is difficult to follow a diet based on a list of foods to avoid and the last thing you need is a difficult stressful task added to your life. Here is a “Yes” list of foods you can eat. It was created by a patient who is also a nutritionist to save others the stress of following the “No” list. The “Yes” list will make it easier to shop and plan your diet.
Patients with daily migraine symptoms have so much abnormal brain activity that avoidance of a few key trigger foods like coffee, red wine, and chocolate is not enough to bring relief. They may continue to suffer despite medications to elevate the migraine triggering threshold. Most of these patients can find relief if they protect their sensitive brains from all potential migraine triggers. This relief does not come instantly. It may take months for daily symptoms to decrease and to allow some good days. With time the good days will increase in number. Be patient.
The migraine diet is not a calorie restricted diet. You can eat as much as you want of the above meals. It is probably better not to be hungry since hunger will lead you to make bad food choices. Eat something sweet for dessert so your sugar craving is satisfied. While the migraine diet is adaptable to a weight loss program, it is best not to diet in the first month as you learn how to eat migraine-free.
Will I need to eat “migraine free” forever? No. Once your sensitive brain has calmed down you can decide with your physician to start adding foods back to your diet in an organized way that allows you to find out which foods are “key” triggers for you and which are “potential” triggers. Key triggers will elicit migraine symptoms within 2 days of being introduced and should be avoided.
Contents
- Migraine Safe Foods by Category
- Acceptable Products for the Migraine Diet
- Tips for Eating Out
- Your First Trip to the Grocery Store
- Menu Plan
- Meal Ideas
- Recipes
- Your Suggestions
Migraine Safe Foods by Category
BREAD
Acceptable purchases - Any white, wheat, rye or pumpernickel store-bought bread.
Plain or sesame seed bagels, English muffins, quick breads like pumpernickel or zucchini breads.
All yeast bread must be 24 hours old.
What to avoid - Fresh baked bread, either homemade or from the grocer’s bakery, fresh donuts, fresh breakfast Danish, nut breads, cheese bread, chocolate bread, raisin bread, bagels with dried fruit like blueberry or cranberry bagels. Remember that pizza is fresh bread.
CEREAL
Acceptable purchases - Many cereals are fine. For example: Cheerios, Life, Honey Bunches of Oats, Cracklin’ Bran, Frosted Flakes, Frosted Shredded Wheat.
What to avoid - Cereal with nuts, raisins, chocolate, dried fruit, aspartame, peanut butter or coconut.
CRACKERS
Acceptable purchases - Any unflavored cracker such as Saltines, Ritz, Wheat thins, Carr’s Table Crackers and Club crackers.
What to avoid - Cheddar cheese crackers, Chick-in-a-bisket, any flavored cracker.
PRETZELS/CHIPS
Acceptable purchases - All plain pretzels and plain potato chips, Tostitos 100% corn chips, Frito’s corn chips, Herr’s salt and vinegar chips.
What to avoid - Soft pretzels, honey and mustard pretzels, onion and garlic pretzels or other seasoned pretzels. Avoid Pringles, Doritos Nacho chips, jalapeno chips and most other seasoned chips.
PIES/CAKES/COOKIES/CANDY
Acceptable purchases - Blueberry and apple store bought pies if made without lemon juice, vanilla or cinnamon swirl cake, shortbread cookies and vanilla/strawberry wafers, oatmeal cookies without the raisins, rice pudding (no raisins), white chocolate.
What to avoid - Chocolate, chocolate candy, nuts, buttermilk, sour cream, dried fruit (some apricot pies start with dried apricots), peanut butter, lemon extract or lemon juice, almond extract and coconut. Avoid diet and sugar-free products that contain aspartame.
SALAD DRESSING
Acceptable purchases - Any oil and distilled white vinegar. (Homemade ranch is good but you won’t find that in the grocery store).
What to avoid - most bottled dressings have one or many of the following; monosodium glutamate, onion or onion powder, grated cheese like Romano or parmesan, natural flavoring, red wine vinegar or balsamic vinegar (or anything other than white).
DIPS/SAUCES
Acceptable purchases - buy ingredients to make your own at home.
What to avoid - dips and sauces usually contain MSG (natural flavoring) or onions. Avoid salsa, chips dips, tomato sauce like Ragu, alfredo or pesto sauce, gravy, mustard dips, barbeque sauce and guacamole (because of the avocados).
MEAT AND MAIN MEALS
Acceptable purchases - Fresh chicken, beef, veal, lamb, fish, turkey or pork. (Some sausage is made without MSG, natural flavor or onion). Be sure the meat is not injected with a tenderizer (like Hatfield’s Simple Tender pork products) or with broth (some turkey and chicken).
What to avoid - Beef liver and chicken liver, marinated meat, ready-made hot wings, barbeque chicken, breaded meat like fried chicken or nuggets or breaded chicken patties, seasoned rotisserie chicken, and any ready-made meal of meat, noodle or rice like burritos, lasagna, Rice-a-Roni and Hamburger Helper. Any canned tuna with broth. Anchovies. Spam. Canned soups have MSG and sometimes onions. Avoid nitrites in ham, hot dogs and most lunchmeats.
DAIRY PRODUCTS
Acceptable purchases - Deli American cheese, American cheese with jalapeno peppers, cottage cheese, ricotta cheese and cream cheese. White milk is ok.
What to avoid– Aged cheeses like Cheddar, Monterey Jack, Colby and Swiss. Avoid mozzarella cheese, Brie, sour cream buttermilk and yogurt. Beware of products made with cheese like pizza and hot pockets. Avoid chocolate milk due to the caffeine.
FRUITS/JUICES
Acceptable purchases - Fresh strawberries, apples, pears, grapes, peaches, nectarines, blueberries, kiwi, apricots, blackberries, cherries, cantaloupes, mangoes, honeydew melon and watermelon.
What to avoid - Bananas, oranges, grapefruit, lemons, limes, tangerines, pineapples, Clementine’s, raspberries, plums, papayas, passion fruit, figs, dates, raisins and avocados. Also avoid dried fruits preserved with sulfites.
VEGETABLES
Acceptable purchases - Preservative-free bagged lettuce like Fresh Express, peppers, zucchini, eggplant, garlic, leeks, spring onions, shallots, potatoes (fresh), some frozen mashed potatoes, broccoli, asparagus, cauliflower, brussel sprouts, carrots, corn, chick peas, mushrooms, canned or frozen peas, yams, string beans, artichokes, red beets, some beans, okra, plain rice, turnips and squash.
What to avoid - Onions, sauerkraut, pea pods, broad Italian beans, lima beans, fava beans, navy beans and lentils. Also avoid boxed potato flakes, like instant mashed potatoes.
DRINKS
Acceptable purchases-Naturally decaffeinated coffee or tea, caffeine-free herb tea like chamomile, pear juice, apple juice, grape juice, cranberry juice, apricot nectar, caffeine-free Coke/Pepsi, Diet Rite Cola, Waist Watcher Cola/Diet Rootbeer/Diet Black Cherry, Mug Rootbeer, Hires Rootbeer and A&W Rootbeer. Diet soda using sucralose (Splenda) is not a problem. Vodka is the best tolerated alcoholic beverage. White milk is ok.
What to avoid - Coffee, tea, coffee substitutes, hot chocolate, colas, orange soda, lemon lime soda, mountain Dew, any diet soda containing aspartame or saccharin, Barq’s Rootbeer, (they add caffeine to it), chocolate milk, wine, champagne, beer, heavy alcoholic drinks.
NUTS/SEEDS/POPCORN
Acceptable purchases - Unflavored popcorn that you pop at home, pumpkins seeds, sunflower seeds without natural flavor, sesame seeds and poppy seeds.
What to avoid - Cheddar cheese popcorn, some microwave popcorn, all nuts and nut butters, including peanuts. Coconut is out as well as almond extract.
SOY PRODUCTS
Acceptable purchases - Any soy is questionable, so you might want to avoid it altogether until you have achieved headache control. Then try the following products one at a time: soy milk, soy flour, plain tofu and soy oil.
What to avoid - Soy sauce, miso, tempeh, soy burgers, products containing soy protein isolate or concentrate and soy beans.
Acceptable Products For The Migraine Diet - a Partial List
- Cereals-Cheerios, Life, Uncle Sam, Great Nuts, Cornflakes. Try Grape Nuts hot: 1/4 cup grape nuts, 3/4 cups milk, plus frozen blueberries. Microwave 2 minutes on high. Add sugar to taste.
- Smucker’s Blackberry Jam - this is important for those of us who previously used raspberry jam. Strawberry and grape are also allowed but blackberry is less ordinary!
- Miss orange juice? Try a product by V8 Splash called Mango Peach.
- If you eat lunch at work, you can bring chicken salad made from canned chicken breast. ‘Sweet Sue’ and some others make canned chicken without MSG.
- Watch out for Hatfield pork products called Simply Tender. These products are tenderized with a lemon juice marinade.
- Dipping mustard for pretzels - Bookbinders hot and sweet works. They use white vinegar and no monosodium glutamate.
- Sunflower seeds - A company called “Here’s Howe” makes sunflower seeds without MSG. Watch out for Planters brand (they use MSG).
- Soda - Caffeine-free and no aspartame: Diet Rite cola, Waist Watcher’s cola, diet rootbeer and black cherry, Mug/Hires/A&W Rootbeer, caffeine-free Coke/Pepsi.
- Miss croutons? Try La Choy Chow Mein Noodles on your salad. Homemade croutons are great too but La Choy Noodles are convenient!
- For another convenience item try Kellogg’s Cornflake crumbs to replace MSG laden breadcrumbs. Homemade breadcrumbs are ok too.
- If you cannot give up coffee and tea altogether be sure you are using naturally decaffeinated products such as Lipton’s naturally decaffeinated green tea or Taster’s Choice naturally decaffeinated instant coffee. If the product just says decaffeinated, most likely a chemical has been used in the decaffeinated process that has been known to cause headaches. Limit even naturally decaffeinated products to one cup a day. I generally drink the Lipton tea and reuse the teabag for a second cup.
- If a recipe calls for buttermilk, substitute 1 cup milk plus 1 Tbsp vinegar. Also, vinegar added to cream cheese can be used in place of sour cream.
- Lettuce can be a problem if it is displayed in a case that sprinkles with what appears to be water on the lettuce. That water sometimes contains a sulfite preservative and should be avoided. This sulfite preservative is also used on salad bar lettuce. I use Fresh Express bagged lettuce. It is preservative-free and convenient.
- Bumble Bee tuna just came out with a new tuna that has no soy or vegetable broth or hydrolyzed protein. It is a ‘prime fillet white albacore in water’. Look for the black and gold can.
- Dried fruit - Many dried fruits use a sulfite to keep the fruit from turning brown. There are brands: i.e., Mariani, that use sulfur dioxide to retain color. This should be ok.
- Canned tomato products - Contadina makes three products without natural flavor (MSG) added: Diced tomatoes, crushed tomatoes in puree and tomato paste. These work well in cattiatore and homemade spaghetti sauce. I have not found any canned or jarred tomato sauce without nature flavor.
- Caramels are a fast and easy treat.
- Ice Cream and toppings - Breyer’s extra creamy vanilla and Breyer’s strawberry ice cream are good choices for the connoisseur, though other brands are ok. Smucker’s dulce de leche (caramel) topping is ok. Also, you can buy frozen strawberries in heavy syrup, defrost and use on vanilla ice cream. It’s not chocolate but it’s better than plain vanilla!
- Bagels - Bagel shops and grocery stores make their bagels daily and that fresh yeast is just a real headache. Try Thomas’s New York Style Bagels, either plain or with sesame seeds. They taste fresh, they are a good size, and they freeze well.
- American cheese - I’ve tried Clearfield and Land-O-Lakes. Both are ok.
- Lunchmeat - Carolina makes ‘just perfect turkey breast’ with turkey and salt as the only ingredients. It is the only lunchmeat I found without nitrites or MSG. It can be frozen in sandwich serving size if you pack a lunch frequently.
- Refried beans for tacos - El Rio makes refried beans that have no onions or MSG added.
- Cookies - Homemade are great if you have the time. Try Keebler’s Sandies Swirl Cinnamon Shortbread cookies for that homemade taste without the fuss. Some vanilla crème wafers are ok too. Beware of cookies that are made with buttermilk.
- Chips - Regular potato chips are ok, as are Tostitos 100% white corn chips, but stay away from flavored chips and Pringles. Pringles starts their product with dehydrated potato flakes preserved with bisulfite to maintain color. This is not listed on the product because they buy the flakes and do not add the bisulfite themselves. They are only required to list that they do use potato flakes. This is a clue for all boxed mashed potato products.
- Peanut butter - This is out but try homemade sunflower butter as a substitute. Start with 12 ounces of hulled raw sunflower seeds. Roast at 300 degrees for 7-10 minutes. Be careful. Over roasting can make the butter taste burnt and dry. Grind the seeds to a fine powder using a food processor or blender. Add about 1 Tbsp sugar and 1/2 tsp salt. Mix in 1/2 cup vegetable oil until smooth (more if needed). Store in refrigerator. Note: I carried some of this butter with me on a trip out west where refrigeration was not available. Even after 10 days, the butter tasted fine. So, you can at least be comfortable packing a sunflower butter sandwich for lunch. Try marshmallow crème on the sandwich for a Fluffer Sunner!
- Chicken broth - many recipes call for 1/2 cup chicken broth. There are no convenient canned products to help you. Canned broth contains MSG and often onions. I make my own chicken broth twice a year using leeks and then freeze the strained broth in one cup serving sizes. While I don’t like the fuss of homemade broth, it is convenient to have on hand and allows me to use many recipes I’d otherwise have to give up. This same principle applies to homemade spaghetti sauce using the aforementioned Contadina products, leeks and Tbsp of brown sugar to counter bitterness.
- Mayonnaise - A small amount on a sandwich is ok but if you want to make a creamy dressing for salad, it is better to use homemade mayo. Then, to 1/2 cup of homemade mayo, add a dash of garlic powder, Italian seasoning, 1 tsp white vinegar, a 1/8 tsp of finely chopped shallot, salt, and pepper and milk to desired thickness. This is the closest I could get to a ranch dressing
- Ocean Spray makes a Lite Cranberry Juice that uses Splenda. It is only 40 calories per cup and tastes great!
- There is one canned soup we can have: Campbell’s Tomato Soup.
Tips for Eating Out
If you eat at fast food places, I know McDonald’s does not season their burgers with MSG. I’m not sure about their grilled chicken. Mac sauce is out, but quarter pounders and double burgers are ok if you request ‘no onions’. McD’s fries are not seasoned so they are fine and vanilla or strawberry milkshakes are ok too. Same with Wendy’s. Wendy’s chili and taco meat has onions and probably MSG. The lettuce on the salad bar may have sulfites and of course the salad dressing has MSG. Watch the cheese in fast food because it is not best quality American - you can always ask for one slice of cheese instead of two on your burger. If you drink soda you will have to bring your own. Burger King scares me - their website shows that their grilled chicken is seasoned with MSG and so are their French fries. Their burgers are smoked, which isn’t that great either. Stay clear of fast-food soup.
I avoid pizza places and all Italian food places because the sauces contain onion and the bread or pizza crust is fresh baked. Salads are a problem because of the dressing, but can be eaten if they have plain oil and salt and pepper. They don’t usually have white vinegar I’ve discovered.
Sub shops are a problem because of the fresh bread and lunch meat. Subway has grilled chicken on their menu but they season it with MSG. I thought the veggie wrap might work but they use the new low carbohydrate wraps which contain soy protein. When my kids want subs, I eat leftovers. (Be wary about all the new “Adkins diet products).
Stay away from bagel shops for lunch because they bake those yeasty bagels 10 minutes before they serve them. You can buy fresh bagels to bring home and eat 24 hours later.
At Ruby Tuesdays/Friendly’s or other sit-down places, the safest thing is a burger without seasoning or onions and unseasoned fries. You need to be very clear about how you want your burger cooked. If I eat at a fancy place, I order steak that has not been tenderized or seasoned and a baked potato with butter and vegetables. Vanilla ice cream is usually available for dessert. Carry a tea bag to restaurants just in case their tea is not ‘naturally decaffeinated’. Some restaurants will offer a plain chicken breast grilled in butter - that works fine.
Eating out is difficult and therefore has become less of something to look forward to. I can eat so many more things if I can control the preparation that I now prefer to eat at home. As a bonus, I get less calories and eat healthier, save money and get less headaches. Intellectually, it is a no brainer!
Your First Trip to the Grocery Store
(THIS LIST WORKS IN CONJUNCTION WITH THE MENU PLAN)
- Best bet: celestial seasonings chamomile herb tea, more risky: naturally decaf green tea (Lipton) or naturally decaf instant coffee (tasters choice). Most risky: a naturally decaf drip coffee
- Bottled water or soda: mug rootbeer, diet rite cola, caffeine-free coke/Pepsi
- Quality sliced American cheese: land-o-lakes or Clearfield
- Frozen hamburgers (rolls too!), cottage cheese, bumble bee prime fillet canned tuna (no broth added)
- Cereal: life, golden grahams, cheerios, frosted flakes, shredded wheat
- Bagels: (you buy cream cheese too)
- Kellogg’s corn flake crumbs to bread pork chops/chicken fingers etc.
- Pork chops and either a whole chicken or chicken legs/thighs
- Eggs, milk, bread, crackers, apple or pear juice
- Vegetables - frozen broccoli and/or brussel sprouts. Also, fresh baby carrots, fresh tomato, celery, baking potatoes
- Unseasoned frozen French fries: canned corn or canned peas
- Regular plain chips and regular unflavored pretzels, sunflower seeds (no natural flavor), popcorn (not microwave)
- Strawberry or vanilla ice cream. Caramel topping
- Olive oil, distilled vinegar and bagged preservative free lettuce
- Fruit: apples, pears, strawberries or blueberries, grapes and canned peaches/pears
EASY MENU PLAN FOR THE FIRST THREE DAYS
DAY 1
Breakfast:
- Hot chamomile teas with sugar (if desired)
- Life cereal with milk –as many as you like
- A sliced apple
Lunch:
- Grilled American cheese or regular cheese sandwich with lettuce and tomato
- Potato chips
- Caffeine free Pepsi or milk
- Keebler Cinnamon Shortbread cookies
Dinner:
- Roast chicken
- Baked potato with butter and salt
- Steamed broccoli
- Blueberry pie, made without lemon juice
- Water
- Snack: Homemade popcorn
DAY 2
Breakfast:
- Hot chamomile tea
- 2 scrambled eggs with American cheese
- Toast with butter
- Pear or apple juice
Lunch:
- Tuna salad on crackers
- Mug Rootbeer or milk
- Canned or fresh pear
Dinner:
- Breaded pork chops - dip in egg, then Kellogg’s Cornflake Crumbs, then fry in oil
- Canned sweet corn
- Salad with oil, vinegar, salt and pepper
- Water
- Vanilla ice cream topped with caramel sauce
Snack: Sunflower seeds without MSG or natural flavoring
DAY 3
Breakfast:
- Hot chamomile tea
- Sesame bagel with cream cheese (and blackberry jam if desired)
- Milk
- Blueberries or strawberries
Lunch:
- Cottage cheese with canned peaches in heavy syrup
- Petite ready to eat carrots
- Pretzels
- Water, acceptable soda/juice/or milk
Dinner:
- Cheeseburger on roll, with tomato and ketchup if desired
- Frozen unseasoned French fries with salt
- Side salad, if desired
- Leftover blueberry pie from Day 1
- Water
Snack:
- Crackers with jelly or a small bowl of cereal
Meal Ideas
SOME BREAKFAST IDEAS
- Eggs and toast
- Pancakes with acceptable sausage
- French toast with maple syrup
- Minute oat meal with brown sugar
- English muffin with butter and acceptable jelly
- Bagel (no raisins or dried fruit) and cream cheese
- Certain muffins (no raisins)
- Day old Danish/donuts
SOME LUNCH IDEAS
- Grilled American cheese sandwich
- Tuna salad made with acceptable tuna
- Turkey sandwich
- Homemade chicken salad on day old roll
- Homemade soup
- Green salad with acceptable vegetables and homemade dressing
- Homemade egg salad
- Fluffer-sunner sandwich made with sunflower butter and marshmallow
- American cheese with jalapeno peppers on club crackers
- Leftovers from dinner!
SOME DINNER IDEAS
- Chicken parmesan
- Tacos
- Sloppy Joes
- Shepherd’s pie
- Pasty - beef, potato and leek
- Chili - beef or hot sausage
- Chicken Cattiatore
- Chicken pot pie
- Beef stew
- Salmon with cranberry sauce
- Vegetable soup
- Crab corn soup
- Sweet potato soup
- Roast beef with vegetables
- Chicken wings
- Gnocchi with red sauce
- Breaded pork chops
- Chicken tenders
- Steak
- Cheeseburger/French fries
- Angel hair pasta with broccoli and shrimp
- Fish and vegetable medley
- Spaghetti with tomato sauce
- Roast chicken
- Chicken vinegar
- Hot sausage sandwich with green pepper and leeks
- Scallops and asparagus
- Beef stroganoff
- Deep dish pizza
- Pasta with bell pepper and hot sauce
- Crab cakes
- Try breakfast for dinner:
- Pancakes with maple syrup and sausage
- Cheese blintzes with blackberry jelly
- French toast with vanilla and cinnamon
- Cheese and mushroom omelet with toast
- SIDE DISHES
- Baked beans
- Roasted vegetables
- Kugel
- Backed potato
- Mashed potato
- French fries
- Parsley potatoes
- Applesauce
- Sweet potato bake
- Baked corn
- Green bean salad
- Rice
- Buttered noodles
- Cornbread
- Potato pancakes (use shallots)
- Corn on the cob
- Creamed corn
- Scalloped potatoes
- Broccoli
- Cauliflower
- Carrots
- Salad with homemade dressing